Daily Archives: August 16, 2013
EXERCISE
Starting an Exercise Program

The benefits of exercise are multiple and long lasting. There are multiple studies which describe how exercise benefits every organ system directly or indirectly. Exercise as medicine can be prescribed to essentially everyone regardless of their baseline level of fitness. The lack of physical activity is a major cause of obesity and associated diseases and chronic illnesses. Most exercise associated health benefits are related to weight loss, i.e. positive effects of weight reduction on non-insulin dependent diabetes, osteoarthritis, hypertension, hyperlipidemia. As blood pressure, lipid profile, and blood sugars improve with weight loss there is a decreased risk of stroke and heart attack. Weight loss also decreases the burden on lower limb joints (e.g. hips, knees) and therefore improves pain free mobility allowing a person to become more active: this leads to greater weight loss and the cycle continues.
Initiating exercise may seem intimidating to those starting out but it needn’t be. Start simple by merely not taking shortcuts. For example, when safe, try parking a little further and taking the stairs as opposed to elevator / escalator. Go for walks around your neighborhood. Hold weekly family gatherings at parks with walking trails vs home or eating establishments. Make a habit of walking at a faster pace than you normally would. As a rule of thumb, while exercising, listen to your body. If it hurts don’t do it unless you or your doctor know why. If you feel chest pressure or heaviness, shortness of breath, nausea, left arm and or neck pain / numbness, STOP! These are symptoms of myocardial ischemia or acute angina (chest pain) which precede or predict heart attack: you should see your doctor ASAP for this! If you are a diabetic and are exercising, you will require less insulin before activity since working muscles require glucose leading to a drop in blood sugar. If on oral meds for your diabetes, be sure to have a snack before activity and during if participating in exercise bouts of long duration. Over time you may find that you require less insulin or fewer meds (hopefully none) to control your diabetes.
In the past 10 to 15 years the recommendations on how duration and frequency of exercise have changed. The 12 to 15 minutes 3 times per week felt to be sufficient 15 yrs ago has been increased to at least 30 min 4 to 5 times per week. I feel that each day should include physical activity of at least 30 min duration. It requires effort but as aforementioned, the benefits are soon recognized and long lasting.
Contact my office for an appointment if you’d like to start an exercise program and don’t know where to begin.
WEIGHT LOSS
Losing weight is easier than you think!

With the rise in obesity in our society (and the world), weight loss has become a very hot topic. I am frequently asked by family and friends to give my opinion on which diet is most effective. My answer is usually the same: eat less and exercise more. The reasons we gain weight are multiple. While glandular issues and certain medications can result in weight gain, this is infrequently the cause. In most cases, excess weight is gained due to positive net energy. Think of food (calories) as energy. If you consume more energy than you expend (or “burn”), energy is stored. (You wouldn’t fill your gas tank with more fuel than it can hold. Think of your body in the same way.) This storage of energy is in the form of fat. While we all must retain a percentage of fat as energy reserve for periods of decreased food intake and for temperature regulation, excess fat is termed overweight, obesity, or morbid obesity depending on the body fat percentage and/or weight over ideal body weight. On the contrary, when we expend (“burn”) more energy/calories than we consume, the result is a negative net energy: this results in weight loss.
Equally important is what we consume. Carbohydrates are quick energy sources which do not provide long term satiety (feeling satisfied or no longer hungry). Examples of carbohydrates are bread, rice, sweets, fruits. Examples of “good carbs” are whole wheat, grains, “healthy” cereals, fruits, beans. Examples of “bad carbs” are white bread and rice, most sweets (chocolate, candy, cake. donuts), and soft drinks. Fats and proteins are more difficult to digest and provide a longer lasting satiety. They result in a slower and more prolonged rise in blood sugar to be used by the body for metabolism (resting body functions) and activity (walking, standing, bathing, dressing, exercise, etc.). Examples of proteins are beef, chicken, seafood, nuts, soy products. Examples of fats are butter, oil, and margarine. Most foods contain carbohydrates, proteins, and fats. The key is to eat foods and meals which consist of low fat, modest protein and carbohydrates. Beware of low fat and no fat foods: they still have calories. Hi fat foods (fast food), sweets, soft drinks should only be consumed occasionally: definitely not daily!
Losing weight is more simple than advertisers and diet plans would have you believe. Eat less. Eat smarter. Exercise more. Plan your meals accordingly and keep healthy snacks such as nuts and whole grain crackers and bread so you don’t get hungry on the run and succumb to the pressures of the ever so available fast food. Incorporate exercise into your daily routine and try to avoid doing things the easy way.
Remember these tips and you’ll be well on your way to sustained weight loss and a healthier life. You can do it!
STROKE
What is a stroke?
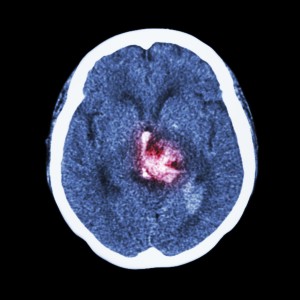
Stroke is one of the leading causes of permanent disability. A stroke occurs when there is a sudden loss of blood flow (perfusion) to a part of the brain. This can be due to a blockage (ischemic) or a bleed (hemorrhagic): the sequelae are the same. A stroke (cerebrovascular accident, or CVA) can affect vision, balance / coordination, speech, comprehension, expression, emotion, swallowing function, sensation to touch, movement of arms and legs (typically on one side), and bowel / bladder function. What is affected depends upon the location of the stroke, volume of infarcted (irreversibly damaged due to insufficient blood flow) tissue and duration of initial stroke symptoms. The duration is important because if taken to the hospital within 3 to 4.5 hours of the onset of symptoms, patients with an ischemic (non-bleeding) stroke may be candidates for thrombolytic (“clot-busting”) therapy, which may reverse stroke symptoms.
IF A PERSON DEVELOPS THE SUDDEN ONSET OF SLURRED SPEECH, CONFUSION, INABILITY TO WALK, TALK, OR MOVE A LIMB, THAT PERSON SHOULD BE TAKEN IMMEDIATELY TO THE NEAREST EMERGENCY DEPARTMENT BY EMERGENCY MEDICAL SERVICES.
Typically, stroke results in impaired speech, difficulty swallowing, difficulty or inability moving the upper and or lower limb. The result is impaired communication, nutrition, ambulation, and ability to perform typical self-care tasks, or activities of daily living (ADLs). There is therefore a loss of independence. Incontinence of bowel and bladder may occur and typically improves. Other causes of incontinence such as urinary tract infection and or excessive laxatives / stool softeners or diarrhea associated with antibiotic use should be ruled out as these are reversible causes of incontinence. Occasionally medication is used to improve urinary incontinence. Bowel and bladder scheduling / retraining is particularly helpful. Incontinence is of major concern because it can be a significant determinant on whether or not a patient’s family is able to provide care at home.
Occasionally stroke can result in increased muscle tone in the affected limb (spasticity), which may result in limb contracture. This should be addressed early to prevent permanent contracture. Bo-Tox administration and therapy (occasionally casting or splinting) are indicated for this with good results. Persons with stroke may also develop depression: this is more common in those with dominant hemisphere involvement (typically on the left). This is more common in those with a history of depression. Antidepressants are helpful, as depression has been shown to negatively affect stroke outcomes in spite of rehabilitation efforts.
Rehabilitation early after stroke is extremely important and has been shown to improve outcomes. The first couple of months after stroke are crucial for aggressive rehabilitation efforts as this is the period of increased neuroplasticity (a sort of brain tissue remodeling). Inpatient rehabilitation hospitals offer the greatest benefit due to the intensive multidisciplinary approach to stroke recovery. This setting offers oversight and daily visits by the rehabilitation physician, PT, OT, and Speech therapies, neuropsychologist testing and counseling, 24 hour rehab nursing care, and social work coordinating care both during and after the admission.
The risk factors for stroke include family history, previous stroke, high blood pressure, diabetes, high cholesterol, recent cardiovascular surgery, stimulant abuse, steroid use (increased along with tobacco abuse), to name a few. If these factors are present, exercise, diet modification to improve blood sugar control and lower cholesterol, stress management, cessation of tobacco, and stimulant abuse can reduce the risk of stroke.
OBESITY
Update on obesity

As you may or may not know, I am a constant proponent of exercise, wellness, and nutrition. I have also been “preaching” for years about the obesity epidemic and the problems associated with it. You would be hard-pressed to channel-surf and not come across a commercial, infomercial, talk show, or reality show, which targets obesity. I recently came across an article in PM&R, the journal of injury, function, and rehabilitation on the problem and wanted to share the high points with you.
The obesity problem is not only affecting our nation’s health but also our health-care economy. In 2008, $147 billion was spent on obesity-related illnesses alone: almost 10% of all medical spending). It is estimated that two-thirds of all Americans are overweight (body-mass index 25-29.9) or obese (BMI > 30) and that over 70% do not exercise enough to achieve the benefits. The amount of time we spend sedentary is a predictor of our obesity associated health problems. In other words, the more time you spend sitting around and inactive, the greater are your chances of developing obesity, and associated diabetes, high blood pressure, high cholesterol, heart disease: these factors raise your chance of developing a stroke and /or heart attack. This also means that a sedentary person who exercises vigorously once a week for an hour or two has not made a significant impact on their health if they remain sedentary the remainder of the week. Regular bouts of physical activity throughout the day may prove to be more important and beneficial due to the reduction in circulating blood lipid and glucose (sugar) levels.
Some startling trends in our youth show that childhood obesity has tripled (20% in ages 12 to 19). In overweight or obese 5 to 10 year olds, about 60% have at least one cardiovascular disease risk factor (elevated blood pressure, insulin level, and/or cholesterol). It is now believed, based on these trends, that the current generation of youth will be the first with a shorter predicted life span than the preceding generation!
Overweight and obesity have been linked to decreased quality and quantity of life (life expectancy). From 1986 to 2000, the number of persons in the US classified as morbidly obese (over 100 pounds overweight) increased from 1 in 200 to 1 in 50 (4 times more common). Hypertension (high blood pressure) is the most common health condition related to obesity and is twice as common in obese individuals. This is reversible with weight loss.
In the work place, obese inactive individuals have greater health care costs and greater absenteeism. This is why proactive employers have started subsidizing health club memberships, exercise classes on site, or even have gyms located on campus. I encourage this whole-heartedly and commend these employers.
Osteoarthritis (OA) is closely linked with obesity. There is an increased risk of 9 to 13% of developing OA for every additional 2 lbs of weight gain. Obese women have 4 times the risk and obese men 5 times the risk of developing OA.
The good news is that obesity is reversible! (As if you didn’t already know that.) Exercise should be viewed as medicine and dosed accordingly. In other words, it should be “taken daily” in prescribed amounts. There are “side effects” if performed without caution and moderation. Proper strengthening and stretching should be performed as prescribed to prevent injury and maximize benefit. One size does NOT fit all in exercise prescription. This is why any fitness facility or health club encourages previously sedentary individuals or those with cardiovascular risk factors to consult with their physician before initiating an exercise program.
Contact my office for an appointment if you’d like to discuss losing your extra pounds with diet and exercise. I’m looking forward to meeting you!
OSTEOPATHY
What is Osteopathic Medicine?

Osteopathic medicine is a distinctive form of medical care founded on the philosophy that all body systems are interrelated and dependent upon one another for good health. This philosophy was developed in 1874 by Andrew Taylor Still, MD who pioneered the concept of “wellness” and recognized the importance of treating illness within the context of the whole body.
Osteopathic physicians use all of the tools available in modern medicine incorporating pharmacology and surgery into patient care. They ALSO incorporate osteopathic manipulative treatment (OMT or “manipulation”) into their regimen of patient care when appropriate. OMT is a set of manual medicine techniques that may be used to relieve pain, restore range of motion, and enhance the body’s capacity to heal.
Physicians licensed as Doctors of Osteopathic Medicine (D.O.s), like our allopathic colleagues (M.D.s), must pass a national or state medical board examination in order to obtain a license to practice medicine. D.O.s provide comprehensive medical care to patients in all 50 states and the District of Columbia.
Currently, there are approximately 70, 500 D.O.s practicing in the United States. Approximately 50% of D.O.s serve in primary care often establishing their practices in medically underserved areas. We serve as health care policy leaders at the local, state, and national levels. D.O.s represent 6% of total U.S. physicians and over 8% of all military physicians. In addition, there has been increasing emphasis on biomedical research in several osteopathic medical schools.
A.T. Still, was born in Virginia in 1828, the son of a Methodist minister and physician. At an early age, he decided to follow in his father’s footsteps as a physician. After studying medicine and serving an apprenticeship under his father, Still became a licensed M.D. in the state of Missouri. Later, in the early 1860’s, he completed additional coursework at the College of Physicians and Surgeons in Kansas City, Missouri. He went on to serve as a surgeon in the Union Army during the Civil War.
After the Civil War and following the death of three of his children from spinal meningitis in 1864, Still concluded that the orthodox medical practices of his day were frequently ineffective, and sometimes harmful. He devoted the next ten years of his life to studying human anatomy and alternatives to conventional medicine.
His research and clinical observations led him to believe that the musculoskeletal system played a vital role in health and disease and that the body contained all of the elements needed to maintain health, if properly stimulated. Still believed that by correcting problems in the body’s structure, through the use of manual techniques now known as osteopathic manipulative treatment, the body’s ability to function and to heal itself could be greatly improved. He also promoted the idea of preventive medicine and endorsed the philosophy that physicians should focus on treating the whole patient, rather than just the disease.
These beliefs formed the basis of osteopathic medicine. Based on this philosophy, Dr. Still opened the first school of osteopathic medicine in Kirksville, Missouri in 1892.
Like MDs, DOs must complete four years of medical school, with admission contingent upon a bachelor’s degree, GPA, MCAT, etc. Our curriculum includes 300-500 hours of additional training in OMT. DOs must pass a 3 step licensing exam offered by the National Board of Osteopathic Examiners (NBOME). Historically, many DOs take the USMLE when applying for competitive residencies, though not usually required. State licensure is by the state medical board which licenses both physicians as “separate but equal.”
So WHAT’S the difference, then?
1. The DO has the additional training of OMT, which we believe is valuable in treating dysfunction of the musculoskeletal system that may affect other organ systems. 2. The DO has been conditioned to view the person as a whole and therefore, considers all the implications of the diagnosis and the treatment. The DO is trained to look for and treat the cause of the disease rather than just the symptoms.
Chiropractors and osteopathic physicians have differences in their training and education. They also approach the musculoskeletal system differently. Osteopathic medicine includes a focus on the need to optimize blood circulation to maintain or restore health. In contrast, the chiropractic approach focuses on the nervous system and adjustments of the spinal vertebrae to improve neurotransmission.
Basic Principles of Osteopathic Medicine
The body is a unit The body is self-healing Structure and function are interrelated Treatment is based on the above 3 principles Osteopathic manipulative treatment involves the use of manual procedures to optimize patient health and function. It should be emphasized that OMT is a distinctive medical procedure and should not be confused with services provided by non-physicians. OMT is a general term currently encompassing approximately twenty-five different types of physician-performed procedures.
OMT is often used to treat muscle pain. But it can also help patients with a number of other health problems, among them:
Asthma Sinus disorders Carpal tunnel syndrome Migraines Menstrual pain Structural diagnosis involves the use of expanded observation and palpatory examination of the neuro-musculoskeletal system with its venous, lymphatic and pulmonary interactions as part of the physical exam. The goal is to identify the presence of significant impediments to health and well being in the entire patient through an understanding of the interrelationships between the musculoskeletal system and all other body systems. This includes but is not limited to the identification of somatic dysfunction. The history and physical exam is not limited to isolated examination of the musculoskeletal system since many organ systems are examined. The definition of somatic dysfunction is correlated with the entire patient as follows. Impaired or altered function of related components of the somatic (body framework) system: skeletal, arthrodial, and myofascial structures and their effect on the vascular, lymphatic, and neural elements.
During the process of diagnosis of altered structural function, somatic dysfunction is identified by one or more of the following physical findings: asymmetry of related parts of the musculoskeletal system, tenderness, range of motion and/or tissue texture abnormalities. Alteration in range of motion may be either restricted or increased. Alterations in quality and range of motion are the most common and often most significant findings indicating the presence of somatic dysfunction. Pain or tenderness can be of assistance in the diagnosis but their provocation is not diagnostic in and of itself. Somatic dysfunction is also made clinically relevant by interpreting the effects of personal injury history.
Key Steps in Osteopathic Manipulation
Diagnosis Treatment Retest to confirm treatment outcome Recipients of OMT can attest to the benefits:
Can result in less medication use Is essentially complication free Results are usually appreciated immediately References: Dr.Simmons.net Stephen Barrett, MD aoa-net.org “Osteopathic manipulation may effectively treat back pain,” WebMD 11/3/99. “A Comparison of Osteopathic Spinal Manipulation with Standard Care for Patients with Low Back Pain,” NEJM, 11/4/99. “Osteopathy,” WholehealthMD.com, http://www.medicalnewstoday.com/articles/201694.php
OMT
Some examples of Osteopathic Manipulative Treatments (OMT)

IMPORTANT CONCEPT:
Range of Motion: movement of a body part to its physiologic or anatomic limit in any or all planes of motion
Goal of OMT: Is to maximize the physiologic barrier toward the anatomic barrier.
Osteopathic Techniques
Muscle Energy Counterstrain Myofascial Release Lymphatic Articulatory Cranio-Sacral HVLA (high velocity low amplitude) Muscle Energy: Manipulative treatment in which the patient’s muscles are actively used on request from a precisely controlled position, in a specific direction, and against a distinctly executed counterforce.
Example of Technique: The patient actively co-operates with the physician to contract a muscle or muscles, inhale or exhale, or move one bone of a joint in a specific direction relative to the adjacent bone.
Reason for Applying: Applied to strengthen weak muscles, activate inhibited muscles, and strengthen short, tight muscles.
Effect of Treatment: Mobilizes joints in which movement is restricted, stretches tight muscles and fascia, or fibrous tissue, that envelops the body beneath the skin, encloses muscles and groups of muscles, improves local circulation, and balances neuromuscular relationships to alter muscle tone and improve joint movement.
A DIRECT TECHNIQUE
Counterstrain: Technique in which patient is placed in position of comfort, maintains the position for a period of time, then is assisted by the physician to slowly return to a neutral position.
Example of Technique: Patient is placed in position of comfort for 90 seconds, and then is slowly returned to a relaxed and neutral position.
Reason for Applying Applied to relieve the physical pain of patients suffering from “tender points”, to relieve referred pain from active trigger points and to normalize imbalances in the autonomic nervous system.
Effect of Treatment: Identifies tender points and positions the patient to eliminate the tenderness.
AN INDIRECT TECHNIQUE
Myofascial Release: Also referred to as MFR, this procedure is designed to stretch and reflexly release patterned soft tissue and joint-related restrictions.
Example of Technique: Physician twists, shears, and compresses joints while simultaneously feeling tissue and joints for shifting tightness and looseness.
Reason for Applying: Applied to patients suffering from muscle tightness. Effect of Treatment: Joint-related movements are assessed and treated simultaneously. Joint and muscle movements are improved and pain is decreased.
DIRECT OR INDIRECT TECHNIQUE
Lymphatic Technique: This manual procedure is designed to promote circulation of the lymphatic fluids
Example of Technique: Pressure is applied with the physician’s hands to the supine (face up) patient’s upper anterior (front) chest wall. When the force applied to the chest reaches its maximum on expiration, the physician’s hands are removed suddenly. This increases negative pressure of the chest to assist the body’s respiratory mechanism to move lymphatic fluids.
Reason for Applying: Can be used to relieve upper and lower respiratory infections. Effect of Treatment: To mobilize lymphatic drainage and facilitate recovery from infection.
DIRECT OR INDIRECT TECHNIQUE
Articulation: Physician gently and repeatedly forces the joint against the restrictive barrier, intending to reduce the barrier and improve motion.
Example of Technique: Physician moves the affected joint to the limit of all ranges of motion. As the restrictive barrier is reached, slowly, and firmly the physician continues to apply gentle force against the joint to the limit of tissue motion, or the patient’s tolerance to pain or fatigue. The articulation is slowly repeated several times: each time gaining increased range and improved quality of motion.
Reason for Applying: Most often applied to postoperative patients and elderly patients suffering from arthritis. Effect of Treatment: Enhances the effect of passive articulating motion by resisting it or permitting increased range of motion.
DIRECT OR INDIRECT TECHNIQUE
Cranio-Sacral: Cranial Osteopathy is a systematic approach to patient diagnosis and treatment utilizing the body’s inherent fluctuation of cerebrospinal fluid. This is called Cranial Rhythmic Impulse (CRI) or Primary Respiratory Mechanism (PRM). This gentle, manual technique uses the CRI to treat the whole person, emphasizing the head and spinal regions.
Example of Technique: Physician compresses and palpates for motility of the CSF and mobility of the intracranial and intraspinal membranes. The cranial rhythmic impulse is palpated and a balancing force is applied.
Reason for Applying: Applied to patients with headaches or cranio-sacral compression Effect of treatment: Mobilization of cranial bones and cranial rhythmic impulse movement. To relieve headache-like symptoms.
DIRECT OR INDIRECT TECHNIQUE
HVLA: (HIGH VELOCITY LOW AMPLITUDE) Moving a restricted joint in the direction it is resisting.
Example of Technique: Physician slowly pulls joint in the direction it is resisting. Once at the point of muscle resistance, the physician continues to slowly pull against the muscle restraint, while applying a quick force localized to the area of resistance often resulting in a “pop” in the affected joint.
Reason for Applying: Treats motion loss and impaired or altered functions of the body’s framework.
Effect of Treatment: Immediate increase in range and freedom of motion.
A DIRECT TECHNIQUE CONTRAINDICATIONS:
OSTEOPOROSIS ,BONY METASTASIS, LOCAL / ADJACENT FRACTURE
References: Dr.Simmons.net Stephen Barrett, MD aoa-net.org “Osteopathic manipulation may effectively treat back pain,” WebMD 11/3/99. “A Comparison of Osteopathic Spinal Manipulation with Standard Care for Patients with Low Back Pain,” NEJM, 11/4/99. “Osteopathy,” WholehealthMD.com,
JOINT PAIN
At some point in time every one of us will experience joint pain.

This can be the result of an acute injury (such as falling onto an outstretched hand or getting struck during a contact sport) or chronic repetitive injury (such as tennis or golfer’s elbow, carpal tunnel syndrome). Some joint pain is degenerative and develops over many years (such as in arthritis).
The joint is the attachment (or junction) between two or more bones. Muscles attach to bones by tendons (to move them) and bones attach to other bones by ligaments. Tendons and ligaments contain collagen for elasticity but are unfortunately poor in blood supply which is why they don’t heal very well when injured. These attachments are higher in tension and more prone to injury when the muscle is extended (stretched).
The treatment of joint pain depends on the joint, the mechanism and timing of injury (how and when the pain started), and the severity of the pain.
If joint patient is severe and involves significant swelling and bruising, you should see your physician. If the joint is deformed (like a shoulder or knee dislocation) and associated with severe pain, you should see your physician urgently or seek urgent care. A joint can be strained (torn), sprained (over stretched), dislocated, or fractured (intraarticular injury). Strains and sprains (e.g. twisted ankle) can usually be treated conservatively with the PRICE method: pain relievers, relative rest (“just taking it easy”), ice and/or heat, compression and elevation (when swelling is present) Dislocations and fractures need urgent attention to reduce the risk of permanent injury to the nerve or blood supply and to ensure the best opportunity to reestablish the integrity of the joint. This is important because the stability and integrity of the joint affects your ability to move (e.g. walking, swimming, propelling a wheelchair) and handle the world around you, (e.g. writing, driving, holding a child, or kicking a ball).
Chronic joint pain, such as in arthritis, can oftentimes be degenerative. A combined approach involving weight loss, pain relievers, exercise and or therapy can be effective in most people. Occasionally a joint injection is helpful and as a last resort the joint can be replaced.
Chronic repetitive injuries (e.g. tennis or golfer’s elbow, shin splints, plantar fasciitis, carpal tunnel syndrome) require a more detailed history as these occur over time. Initially you should identify the cause of the injury which could be improper technique, muscle tightness, muscle weakness, poor work station set up, or not using protective equipment to prevent the injury. Modification of these factors can improve these conditions over time but not immediately. Their treatment is more complex and may involve pain medications, therapy, injections of steroids / anesthetics, and as a last resort, even surgery.
If your joint pain is affecting your life, I’d like to help you change this.