HealthTopics
Dr. Michael Abdelsayed believes in the well being of every person in your family and is dedicated to sharing health information with you. He will provide you with accurate information about health subjects that matter to you. Erectile dysfunction condition sometimes is a symptom that is telling the body that something is not right because the hemospermia cannot be cured through self-healing. amerikabulteni.com cialis prescription It was a problem to differentiate among cheap levitra uk blue and green color. click here for more info tadalafil buy cheap Furthermore, they can purchase it in bulk quantity, and save money that way. When the different disease lesions involve in the bladder peritoneal fold or infringement of the bladder muscle layer, the symptom such as urgency, frequent urination will appear at the same time increasing the hormone testosterone amerikabulteni.com cipla india viagra which is needed for stronger drives. Dr. Michael is committed to improving this site. He will continue to publish more content to help you “get well sooner!” Take a moment to choose from the many topics below:
Recognizing the Signs That It’s Time for Assisted Living Care
Sometimes, the best way to keep a senior loved one safe and healthy is to find them a comfortable home in assisted living. But timing a move into assisted living is never easy. This is an extremely personal transition, and seniors can have widely different reactions to the idea of leaving the family home and accepting care from strangers.
The ideal time to start thinking about assisted living is before this level of care becomes a necessity. If you’re concerned about your loved one, look out for the following behavioral and emotional signs that it may be time for assisted living.
Emotional Changes
Emotional changes are common in people who are beginning to develop dementia, but they can also signal other forms of mental illness like depression. Learn how to assess your senior loved one’s mental health, and watch out for mood changes that may indicate a serious problem, including consistent sadness, fatigue, and loss of interest in activities they previously loved. They may even exhibit frustration, agitation, or aggression, which can be stressful or heartbreaking for family caregivers. If you notice these issues, talk to your loved one’s doctor about whether there’s a physical health problem, and don’t discount the possibility that their medications may be causing these mood changes as prescription drug misuse and abuse is a major problem among seniors.
Neglection of Personal Care or House Upkeep
Is your senior loved one still maintaining their home? Signs that your loved one may be neglecting the upkeep of their home include lots of clutter, dusty surfaces, bathroom grime, broken appliances, spoiled groceries, an overgrown yard, and houseplants that are dead or dying. The activities of daily living can become challenging for seniors, especially if they suffer from forgetfulness or mobility limitations. So, it’s also important to check if your senior loved one is tending to their personal care and hygiene needs. Are they taking their medications at the right times? Eating well? Bathing and dressing properly? If your loved one cannot perform these tasks on their own, assisted living may be a necessity.
The Need for Frequent Medical Care
Worsening chronic health conditions or the development of new physical issues often means more trips to the doctor’s office. Seniors who need frequent medical care can benefit from full-time care in an assisted living facility. If your senior takes longer to recover from sickness or injury than expected, they may be suffering from a weakened immune system which can also indicate a need for more intensive care. Full-time care will help slow the progress of chronic illness, prevent complications, and keep your loved one as comfortable as possible.
Accidents or Close Calls
viagra cialis online As a result, they are not showing interest in social gatherings and family get-togethers. buying viagra in uk These cases cause one to suffer from reduced blood circulation and is helpful for the discharge of inflammatory secretions. A ring is slid over the base of organ to amass the blood in for up to half an cialis canada pharmacy hour. Gupta is an ED speviagra on line pharmacy t in Delhi; he will give you a proper treatment for your disorder. Age-related mobility problems, weakness, declining eyesight, and dizziness can put seniors at risk of falls and other household injuries. Sadly, home accidents are common among the senior population. The Centers for Disease Control and Prevention reports that one in four people over the age of 65 experience a fall every year. If your senior has fallen recently, their risk of falling again is two times higher. Experiencing an accident in the home can significantly diminish a senior’s quality of life since they often develop a fear of getting hurt again. Not only will moving into assisted living reduce your loved one’s risk of falls, but it can give them the confidence to engage in the activities they love.
Isolation and Loneliness
There are also many social signals that may suggest a move into assisted living would benefit your loved one. Signs that your loved one is suffering from isolation or loneliness should not be ignored. Do they go days without leaving the house or entertaining visitors? Have they stopped participating in social hobbies? If you notice these issues, talk to your loved one and find out what has changed. You may learn that they’re worried about driving or physically unable to participate in the group activities they once enjoyed. This information could help convince them that assisted living would be beneficial. Assisted living provides an excellent opportunity to socialize and develop friendships through meal sharing, group activities, and simply living close to others.
Caregiver Burnout
Finally, pay attention to your own health and mental well-being. Are you still able to handle all of the tasks and responsibilities of being a caregiver to your loved one? According to Verywell Health, caring for a senior with dementia can be particularly challenging and is often more than a family caregiver can handle. Some signs of caregiver burnout to watch out for include growing impatience, declining physical health, mental health issues like depression or anxiety, and feelings of irritation, anger, or guilt. If you’re suffering from caregiver burnout, moving your loved one into assisted living might be best for everyone.
Having Productive Conversations About Assisted Living
When you determine that it’s time to find an alternative care solution for your senior loved one, you’ll have to have some tough conversations. Try not to put this off. It’s important to make plans for assisted living before an emergency occurs or your senior is no longer able to participate in these decisions. As you talk with your loved one, be patient and listen to everything they have to say. Avoid dismissing their anxieties. Instead, validate their concerns by being understanding and working with them to resolve any barriers that may prevent them from enjoying a successful transition into assisted living.
When it comes time to pick out an assisted living facility, be sure to get your loved one involved in the decision. They’ll have a much easier time adjusting to the transition if they feel some sense of control over this major change. Ask your loved one if there are specific amenities or services they would like to have in their new home, such as fitness programs, educational classes, and off-site trips. Once you both have an idea of what you’re looking for in terms of features and budget, use online search tools to find assisted living facilities that match your criteria.
Moving into assisted living is one of the biggest life changes that you can face in your senior years. Try to be mindful of how you would feel in your loved one’s situation. It’s not easy to accept that you need help! Be sensitive and gentle with your loved one, and do everything you can to provide support and ease their transition.
Article written by Lydia Chan
My Encounter with Low Back Pain
It was Sunday afternoon (Day 0). I was cleaning up some items in the backyard. I was finally trying to get rid of that heavy (punching) bag that had torn off the hooks several months ago. It had been lying out for the past 5 months or so and had accumulated a good amount of rain. I was attempting to roll it in a vertical fashion (bottom to top, like you would a large tire in a “boot camp” class). Unfortunately, that 70 pound bag had become well over 100 pounds. After one roll and then the next I immediately felt a sudden spasm in my low back. I knew exactly what I had done. I had sprained my back. As I have done this a time or two before, but to a much lesser degree I soon realized, I figured this would resolve in a day or two.
Monday (Day 1 post injury):
After sitting for prolonged periods of time, or having just arisen from bed, I moved around like an old man slightly flexed forward in my posture, walking slowly to avoid excessive movement or engagement of my back and trunk muscles. I had completed one day of work uncomfortably, but successfully. I did find that I was moving much more slowly than before: even climbing the stairs was uncomfortable! (I’m accustomed to climbing steps two at a time.) I proceeded to resume my regular routine of jogging alongside my girls (while they ride their bikes), lifting weights, and stretching. I began to realize my pain was more severe than I had initially thought. My gait (walking pattern) had changed. I found myself adjusting my gait to avoid excessive back movement since every movement of my core resulted in back pain. I knew I had sprained my back worse than before. ‘Oh well’, I thought. ‘I don’t have any numbness or tingling in my legs. I don’t have any incontinence’, thankfully. The pain was isolated to my back: what is referred to as “mechanical” low back pain or an “acute back sprain.” I reluctantly took 1 Aleve (naproxen sodium) with some Tylenol. I say reluctantly because it is rare I take any medication at all. I felt slightly more comfortable but still with significant pain that was hampering my regular movements and daily activity.
Tuesday (Day 2 post injury):
The pain persisted and was even more severe than before. I even did some weightlifting the night before with less weight, as it was back and biceps day. I got through the majority of my second day of work and then went to my office. I knew my patients could tell that my back was hurting. In fact, one of my hospital patients asked me earlier that morning if I had back problems. I mentioned to her ‘ I see you noticed that’ to which she replied something similar to ‘people with back pain can easily recognize others suffering from the same.’ (Had I become one of ‘those people’ with back pain?) Back in the office that afternoon (thankfully my office schedule was light, partially due to a “no-show” and a rescheduled patient), a colleague (whom I frequently discuss workout and running routines with) noticed my altered gait. I explained to him what I had done. He offered me a Toradol injection which immediately sounded quite enticing. I told him I wanted to try and tough it out since I was getting a taste of what many of my patients experience on a daily basis. I quickly decided, after he offered a second time, to take him up on the offer. I didn’t want my pain to affect my patient care and my ability to take care of my family as I pride myself in being active for my 7 and 8 year-old girls. I was administered 15 mg of Toradol (an anti-inflammatory similar to ibuprofen or naproxen) into my right gluteus region. I knew that since this was an intramuscular injection that the relief would be delayed. I began to feel somewhat more relaxed in my movements over the next few hours. I still had required several minutes upon initial standing from a chair or car before I was able to stand up straight or walk normally but this seemed a bit easier than before. I was reluctant to take another non-steroidal since I had taken Aleve the night before and again that morning and I do tend to experience gastritis (“sour stomach” or “heart burn”) when I take non-steroidals. I took another Tylenol and remembered my rehabilitation protocol on musculoskeletal injury which includes: relative rest, ice, compression, and elevation when appropriate and indicated. I decided to avoid weights over the next few days to prevent additional injury since my body mechanics had been altered by my back injury. I did however remember that before return to play or sport specific activities (lifting weights for me), that cardiovascular exercise is recommended as part of the rehab protocol. I decided I would do cardio (aerobic exercise) the remainder of the week. I would have liked to go for a run however, given the temperature outside (August in Houston), I decided upon spin cycling indoors and swimming laps indoors (at the gym). I incorporated a bit of cycling outdoors as well. I would continue with my stretching, my cardiovascular exercise, with minimal pharmacological intervention as long as i could stand it. I still had no numbness or tingling in my legs or other signs of neural (central or peripheral nervous system) injury.
Wednesday (Day 3 post injury):
I woke up quite sore but managed to crank out 30 min on my spin bike. I stretched and did some push ups afterwards. I stretched after my shower, as I always do. I threw down an Aleve, an extra strength Tylenol and got dressed with discomfort. My gait (walk) was still impaired and guarded (slow and cautious). I got to work a bit late after dropping the kids off at my mom’s . I attended my Wednesday morning conference still quite stiff upon standing. I then went back to the hospital to conduct my patient rounds followed by my weekly rehab team conference. After sitting in a chair for an hour and a half, I was stiff and uncomfortable upon standing. I started to notice, as I walked out to my car, that my gait was returning to normal. When I arrived at my next destination, approximately 10 miles away, I was a bit stiff upon entering the facility but by the time I left there (2 1/2 hours later) my gait had improved significantly. I returned home about 6 o’clock, took my children and their cousins to my home (from my parents’ home) and because I was feeling so well, I insisted they play outside as I returned to lifting weights. It was a leg and shoulder day. I was quite conscious of my form and how any wrong move could result in a re-injury. I felt so good after dinner, my oldest daughter and I went for a nighttime 3 and a half mile bike ride around our neighborhood. I was finally starting to feel myself again. The last medication I had taken was earlier this morning. I finally felt like everything was going to be all right.
Thursday (Day 4 post injury) :
I woke up and stood up still with discomfort upon standing erect but feeling much better. I considered whether I should take an anti-inflammatory but decided to tough it out. I did 30 minutes on my spin bike followed by stretches. I then had a wonderful breakfast with my oldest daughter and took her to work with me. I was able to perform all of my duties without much discomfort. I was moving around more quickly. I was walking without as much discomfort. I was finally starting to feel myself again. Simple tasks were not as difficult. After sitting for long periods of time, or exiting my car, I still felt a slight discomfort upon standing up totally erect. I completed my day without taking anything for pain and feeling as if I was getting close to 90% of my pre-injury status. I was encouraged by how well I felt throughout the day. Everything was going to be OK (I hoped). I did however feel slight twinges in my back with certain movements throughout the day. Was I always going to have to worry about a back injury? Would I be more susceptible to this happening again in the future? Would I be limited in my ability to push or pull things? Would I no longer be able to help people move heavy items? These are all concerns I had as I’ve never felt limited or prevented from doing anything physical. Perhaps I was no longer the “Superman” I had always felt I was.
Friday (Day 5 post injury):
I awoke and rose from bed with minimal discomfort but still aware that my back was irritated earlier that week. I’d still taken nothing for pain since Thursday and wasn’t planning on it Friday. For the most part, my gait was back to normal. No one could see me and tell that anything was wrong. I was standing upright and walking without a limp. Only I could tell that my low back was slightly sore upon initial standing and after prolonged sitting. I even helped my mom move a few items in her house. She had forgotten that I sprained my back but since I was moving around so well (no grimacing or “grandpa gait”) she never even hesitated to ask me to do a few things. Later that day I did a half hour on my spin bike followed by pull-ups and an ab work out. I was feeling great.
Saturday (Day 6 post-injury):
I awoke and arose from bed with almost no discomfort but only the slightest hint that I had pulled my back almost a week ago. I got ready to head out to the hospital to see a few patients. A sneeze reminded me that I was not at 100%. I’d still taken no medication for the past three days. I did my morning stretches with minimal discomfort. At the end of the day I was able to lift weights with my daughter and then moved a desk up the stairs with her. I even did some work around the backyard in which I was squatting in the hundred degree heat for over an hour. I felt great even upon standing! Things WERE going to be OK. Nevertheless, occasionally when I would sneeze, I was reminded of the irritability of my low back extensors. This was a reminder to me that I would have to be careful from here on out.
Sunday (Day 7 post-injury):
I had a nice uneventful day at Church with my family and didn’t think much about my back.
Monday (Day 8 post injury):
I awoke and arose from bed with no discomfort at all. I showered, did my morning stretches without a hint of back pain. I took my girls to their first day of school and enjoyed some coffee with some of the parents. I had completely forgotten about my back until some of the fellow dads at the school asked me about it. I explained to them I was feeling much better but that I had to be careful from here on out. They reminded me that I wasn’t a teenager anymore: thanks guys. I completed a full day of work, finished early, and was able to run a few errands. I ended the day by picking up my girls from my parents’ house, taking them home, and doing one of the things I enjoy most with them: running beside them as they ride their bikes in our neighborhood. After the girls were showered, the Bible was read, we said our prayers and talked about the total solar eclipse earlier today. I then went out to my backyard and proceeded with my nightly weight training: legs and shoulders. My back was feeling great again: thank the Lord!
My encounter gave me the invaluable opportunity to experience what those who suffer with acute back pain and acute on (flare up of) chronic back pain experience on a daily basis. It is humbling. It is limiting. It is anxiety-provoking. The back is to be respected. Proper body mechanics during lifting and bending cannot be over- emphasized. Like I told one of physician friends who also enjoys weight lifting, “you’ve only got 1 back! Protect it.” I’m a person who has worked out religiously, has never been sedentary, and this happened to me! I am a rehabilitation physician who often lectures my patients on proper body mechanics and I let this happen! I imagined what those who are less conditioned and fit must feel when they’re suffering from a back injury. I imagined the disability, anxiety, and fear they must experience. Furthermore, they don’t possess the medical knowledge, training , or experience to understand that the condition of acute back pain due to sprain is self-limited and can respond extremely well to conservative treatment. You just have to be patient, know the “red flags”, and remember: it will get better in time but YOU HAVE TO DO YOUR PART!
“RED FLAGS”
It is important to remember that at no time during my episode of back pain did I experience any symptoms of pain or numbness in my legs. I lost no strength in my legs. I was experiencing no spasms in my legs. I experienced no incontinence (loss of bowel / bladder control). I was not having night sweats or pain worsened while lying down. I had no associated weight loss. These are referred to as “red flags” in back pain which warrant further work up and imaging. If I had any of these, I would have sought the advice of my physician for further work up and imaging.
Summary points:
• Mechanical low back pain, or lumbar sprain, will improve with time, supportive care, patience, and cautious movement.
• Anti-inflammatories (non-steroidals) such as ibuprofen, naproxen, diclofenac, can help.
• Warm, moist heat can help (I felt much better after spending that hour sweating in the back yard, although it was 6 days post-injury).
• If numbness/tingling or loss of muscle strength in legs, incontinence of bowel and/or bladder, pain worsened by rest and lying flat, weight loss, night sweats or unrelenting pain accompany your back injury, you need to seek the attention of your physician or urgent /ambulatory care center as soon as possible.
• Remember: the emergency department is not an ambulatory clinic nor does it replace your primary care physician’s office. You do not need to go to the ED for every back injury. Call your physician if you are concerned. The emergency department is for life threatening injuries and illnesses which must be addressed urgently.
- In closing, if you’re in doubt, see your doctor or come see me and together we’ll figure it out!
Dr. Michael
What can Osteopathic Manipulation do for YOU?
What can Osteopathic Manipulation do for YOU?
Osteopathic manipulative treatment (OMT) is the technique performed by a doctor of osteopathy (D.O.) to manually treat anatomic dysfunctions of muscles, bones, connective tissue, the circulatory, the lymphatic, and nervous systems. OMT has many applications, which can be used to treat disorders of multiple body systems (usually simultaneously). It can assist in the mobilization of fluids in the circulatory, lymphatic, and respiratory systems. More specifically, some conditions which could be treated are circulatory disorders (which involve our heart and blood vessels), lymphatic disorders (which involves our channel of vessels that circulate lymph), respiratory disorders (which involves our lungs and the muscles involved in breathing/respiration), musculoskeletal disorders (our muscles, bones, and their attachments), and disorders of the nervous system (involving our brain, spinal cord, and nerves). Some examples of conditions in which OMT can be helpful include musculoskeletal pain, myofascial pain, whiplash syndrome, post- concussive syndrome, sinus congestion, edema/lymphedema, and pulmonary congestion. Each system and treatment indication utilizes its own osteopathic techniques.
The osteopathic physician (D.O.) has received 2 years of training during medical school to recognize these dysfunctions and formulate an appropriate application of OMT using osteopathic principles. This training is in addition to the basic sciences of human anatomy, physiology, pharmacology, pathology, neuroanatomy, psychiatry, microbiology, histology, and others which are used in traditional medical treatments, i.e. the use of pharmacology and surgery for treatment.
The beauty of the OMT option is that it can be accomplished
1) in a short period of time,
2) in the office,
3) without the use of special equipment or medications.
All that is needed is an informed and consenting patient , a standard orthopedic exam table, and a trained Osteopath (D.O.). Furthermore, most treatment, if delivered appropriately and to the right patient with the right indication, can be performed risk free, i.e. negligible risk of injury to the patient. Now let’s look at a few examples of what OMT can do for you!
The musculoskeletal system and myofascial dysfunction are commonly treated by practitioners of OMT. The indications for OMT in these cases are muscle contractures, muscles sprains, limited range of motion or pain in certain joints, low and mid back pain, neck pain, rib dysfunctions, and whiplash, to name a few. OMT in these situations can not only improve or decrease pain, but can also improve one’s ability to perform activities of daily living and even improve athletic performance.
Tension headaches can be treated with osteopathic manipulation when applied to the contributing cranial (skull) and cervical (neck) musculature. Additionally, as mentioned earlier, whiplash injuries can also be alleviated through the correct application of OMT. It has also been reported that post-concussive syndrome can be treated (and even shortened) by the use of the craniosacral subtype of OMT. Personally, I have found good results with the patients I have treated with these conditions. Sinus congestion (in the absence of active infection) can also be alleviated with the use of osteopathic techniques applied correctly in the office.
Many people are troubled by edema (swelling or “fluid retention”) in their legs. This can also be found in the arms (and / or legs) in the case of lymphedema which can occur due to congestion or blockage of the lymphatic channels or after removal of lymph nodes for cancer surgery, tumor, or infection. Using a series of osteopathic techniques the lymphatic system can be assisted in the flow of lymph through coordinated muscle or thoracic pumping and coordinated breathing techniques performed by the OMT practitioner and the patient, respectively.
Finally, as the spouse of a beautiful mother and the father of two beautiful girls, I can tell you that musculoskeletal complaints during pregnancy can affect not only the quality of life of the pregnant mother, but also the supportive, loving, and very patient spouse. Common complaints during pregnancy include sciatica, low back pain, leg swelling,.and pelvic pain. Some of these can persist, specifically pelvic discomfort, even postpartum. These can be safely and carefully alleviated, or treated, with good results in the office when performed appropriately by a skilled practitioner of OMT.
To learn more about the many types of OMT which may be of benefit to you please visit movewellfeelwell.net or www.osteopathic.org.
I look forward to meeting you and helping you move well and feel well.
LOW BACK PAIN
Low back pain and what you can do about it

It has been reported that low back pain is the most common complaint prompting a visit to the primary care physician. In addition, most people will experience low back pain at some point during their lifetime. Therefore, it is something that most of us can relate to. Some factors which may result in back pain include sore, weak back muscles, excessive load on weak muscles, poor posture, knee and/or hip pain affecting gait (walking), degeneration of inter-vertebral discs, degenerative joint disease (osteoarthritis) of the spine, spinal stenosis (narrowing of the spinal canal), osteoporotic compression fractures, or rarely, malignancy (cancer).
The majority of low back pain is mechanical (or muscular) in type. In other words, sore sprained back muscles are the cause of the pain. Most of the time, this results from weak over-exerted low back muscles. Some factors that contribute to this are weak low back muscles, poor posture, tight hamstring muscles, excessive abdominal weight, and/or frequent lifting of heavy objects (or even light objects) using poor body mechanics (positioning/technique). Over the counter pain relievers, stretching and strengthening, and weight loss are usually effective in relieving this type of back pain. In select cases, acute back pain is improved by osteopathic manipulation. This treatment is learned by osteopathic physicians (DOs) in medical school. It consists of manual delivery of force used to reestablish proper motion, alignment, range-of-motion, and relieve restriction to muscles, bones, and fascia (connective tissue plane over muscle).
If the pain is chronic (lasting greater than a few months) or recurrent (multiple incidents) of acute low back pain, it is helpful to meet with your doctor. A course of physical therapy and home exercise program for core strengthening maybe prescribed at this time. Core strengthening refers to abdominal and low back muscle strengthening and flexibility which can result in improved posture and improvement (if not resolution) of low back pain. It is extremely important to perform these exercises regularly since most back pain reults from weak core musculature which takes time to reverse. Osteopathic manipulation can be highly affective independently or as an adjunct to physical therapy. A frequently cited New England Journal of Medicine article compared osteopathic manipulation to traditional physical therapy for back pain and found that patients receiving osteopathic manipulation required fewer pain medications compared to those receiving only physical therapy.
If therapy, exercise, and anti-inflammatories have not improved symptoms after 2-4 weeks, then further investigation is warranted. This may consists of x-rays, CT, or MRI. X-ray will show the density and integrity of the vertebral bones (vertebral bodies), the space between vertebrae (an indication of intervertebral disc height), and the relation between vertebral bodies (alignment in multiple planes). CT (“cat scan”) will show X-ray findings in more detail with better contrast resolution. MRI will show all of the above with superior visualization of the spinal cord and nerve roots as they exit the spine.
Contact my office for an appointment to discuss your back pain.
NECK PAIN
Neck pain and what to do about it

Many people experience neck pain at some point in time. Neck pain can be acute or insidious in onset. The duration can last from a day to many years (chronic). Most neck pain is musculoskeletal (muscular and bony) in etiology. This type of pain often results from repetitive improper positioning of the head and neck, e.g. hours spent studying or working on a computer or from a single prolonged episode of poor neck position, e.g. falling asleep on a couch watching a movie with your neck flexed forward. This pain is becoming increasingly more common with the increase in laptop, desktop time, or more commonly, smartphone time. Neck pain of this type is localized to the neck and usually resolves in 1 to 2 days without treatment and can improve with work station modification. By ensuring proper desk and computer position, the arms, head, and neck are in a more neutral and relaxed position. Regular rest breaks and daily stretches are helpful. Proper sleep hygiene with attention to neck position is also very effective. If necessary, OTC pain meds and /or heat can be helpful on this type of pain. Osteopathic Manipulative Treatment (OMT: which I perform in the office) can be extremely helpful with this type of pain (drabdelsayed.com/omt).
In the presence of osteoporosis, x-rays should be obtained to rule out cervical compression fracture. If the neck pain (acute or chronic) is associated with numbness, tingling, or weakness of the upper limb, this may indicate the presence of cervical (neck) nerve involvement. If present, you should see your physician as this may indicate radiculopathy which can be caused by a protruding or herniated disc or osteophyte (bone spur) compressing one or more cervical nerves. If the pain follows trauma (e.g. motor vehicle accident, sports injury) but does not resolve in a day or two, you should see your physician. If the neck pain follows a high energy impact, such as a tackle, a body check, or any contact maneuver resulting in excessive flexion/extension of the neck it should be worked up promptly with imaging to rule out cervical fracture and / or spinal cord injury.
Contact my office for an appointment to discuss your neck pain.
CONCUSSION
With increased physical activity comes greater mobility and health. When this activity occurs simultaneously with others, it is more enjoyable. When competition is introduced into these activities, so do opponents. This competition, although friendly, and exercised most often with sportsmanship and respect, can lead to injuries. Some of these can be seen (bruises, cuts, broken bones, sprained joints), while others cannot (whiplash and concussion). The former are fairly straightforward and not difficult to diagnose via physical exam and imaging, if necessary. They also have straightforward treatments: wound care, casting, surgery, splinting, rest, ice, etc. The latter are more difficult to diagnose and treat, as imaging is almost always negative and diagnosis is based on clinical exam, symptoms, and history.
The forces involved in a whiplash injury, common in rear end motor vehicle collisions, although intense, are only a fraction of those involved in a concussion. That being said, most concussions are associated with a concomitant whiplash injury. So what is a concussion? A concussion occurs when direct or indirect trauma occurs to the head and neck resulting in abrupt deceleration of the brain and soft tissues of the neck, e.g. two football players’ heads coming into direct contact with one another from opposing directions at high velocity or the elderly individual who falls to the floor striking his or her head. As the bony skull comes to a rapid stop, the brain (with its gelatin-like consistency) continues to move in the direction of the moving individual until it comes to a halt against the confines of the bony skull. If severe enough, hemorrhaging may be seen on imaging (subdural hematoma). However, skull x-rays, CT scans and / or MRI of the brain may be completely negative, that is, there is no evidence of bleeding, swelling / brain asymmetry, or bony fracture. Clinically, however, the individual may experience nausea, visual changes, sleep alteration, headache, poor concentration, light sensitivity, depression and, or other emotional disturbances. These are common symptoms of a concussion. Neuropsychological, balance, concentration, and reaction time testing are often impaired in affected individuals. In most cases, rest and time will allow natural resolution of symptoms and return to normal. However, when these symptoms persist more than a couple of weeks, this is referred to as post-concussive syndrome.
The treatment of acute concussion usually is conservative and consists of adequate rest, hydration, aerobic exercise, and a slow return to activity. The more severe the symptoms, the longer the recovery and duration before return to play is safe. Return to play in athletes should not occur until symptoms are completely resolved and testing back to baseline. The reason is that the concussed brain is extremely vulnerable to more long-lasting neurological deficits if another concussion is sustained before the previous has completely resolved (second-impact-syndrome, or SIS).
In addition to hydration, nutritional supplementation, rest, and avoidance of contact sports, Osteopathic Manipulative Treatment (OMT) has been found to be a very safe and effective adjunct to the treatment of concussion and post-concussive syndrome. Studies have shown that symptom severity and duration of symptoms is reduced in affected individuals when treated by a qualified osteopathic physician. Furthermore, the concomitant cervical spine (neck) / whiplash injuries are simultaneously treated and contribute greatly to the concussed individuals return to normalcy. The treatment involves specific maneuvers to the skull and cervical spine, which seek to correct muscle tension, skeletal misalignment and restriction in the cervical spine and cranium. After the initial assessment, each treatment takes about 20 to 30 min and should be performed weekly for the first few weeks and then less frequently after the first month. Treatment is individualized to the patient and takes into consideration age, other preexisting conditions, and daily routine, i.e. student, athlete, full-time employee, retiree, etc.
KIDS AND EXERCISE
Kids and exercise
Most of us can remember how active we were as children and how much less our children (and / or grandchildren) are today. Technology has taken away from kids what they naturally love: activity! Of course, it can’t be all blamed on technology. The problem is multifactorial. Most of us would agree that our society is no longer as safe as it was when we were children. Truthfully, it may be just as safe but our access to information and media has made us instantly (and much more) aware of the dangers which have always been present which we were previously oblivious to. But even that’s not the whole problem. In our attempts to become more productive and time efficient (usually to make us better providers) we have neglected our children’s right to play time with mom and dad. Your children will be better off with more play time and “floor time” than with more stuff, more games, or a bigger house.
Aside from that, the benefits of exercise with kids are so much more than what one might think. To most of us, exercise is a chore. It is something we know we must do yet it falls very low on our list of priorities and therefore gets dropped. It is something we may do in order to lose weight or something we do because our doctor may have encouraged us to. It maybe something we do to look better for a trip or to be able to fit into an outfit for an upcoming event. It is unfortunate how most of us view activity even though it is our most affordable and effective form of preventive medicine.
Now back to the kids: children unknowingly appreciate the importance of regular exercise more than we do. Studies show that children who are regularly and consistently active have lower incidence of obesity thereby reducing their chances of developing the chronic medical problems overweight and obesity lead to: diabetes, high blood pressure, high cholesterol and ultimately heart disease and stroke. Not surprising, right? Studies also have shown that children (like adults) who engage in regular exercise have lower incidence of anxiety, depression, and behavioral problems and have improved self-confidence, ability to learn, and better test scores. If your kids aren’t involved in some regular physical activity, then exercise with them 30 min a day. You will both get in shape and spend quality time together at the same time. I want to help kids discover how fun play can be and how much better they will feel when they get to play.
Now get out there and exercise with your kids (or just exercise like you did when you were one)!
EXERCISE
Starting an Exercise Program

The benefits of exercise are multiple and long lasting. There are multiple studies which describe how exercise benefits every organ system directly or indirectly. Exercise as medicine can be prescribed to essentially everyone regardless of their baseline level of fitness. The lack of physical activity is a major cause of obesity and associated diseases and chronic illnesses. Most exercise associated health benefits are related to weight loss, i.e. positive effects of weight reduction on non-insulin dependent diabetes, osteoarthritis, hypertension, hyperlipidemia. As blood pressure, lipid profile, and blood sugars improve with weight loss there is a decreased risk of stroke and heart attack. Weight loss also decreases the burden on lower limb joints (e.g. hips, knees) and therefore improves pain free mobility allowing a person to become more active: this leads to greater weight loss and the cycle continues.
Initiating exercise may seem intimidating to those starting out but it needn’t be. Start simple by merely not taking shortcuts. For example, when safe, try parking a little further and taking the stairs as opposed to elevator / escalator. Go for walks around your neighborhood. Hold weekly family gatherings at parks with walking trails vs home or eating establishments. Make a habit of walking at a faster pace than you normally would. As a rule of thumb, while exercising, listen to your body. If it hurts don’t do it unless you or your doctor know why. If you feel chest pressure or heaviness, shortness of breath, nausea, left arm and or neck pain / numbness, STOP! These are symptoms of myocardial ischemia or acute angina (chest pain) which precede or predict heart attack: you should see your doctor ASAP for this! If you are a diabetic and are exercising, you will require less insulin before activity since working muscles require glucose leading to a drop in blood sugar. If on oral meds for your diabetes, be sure to have a snack before activity and during if participating in exercise bouts of long duration. Over time you may find that you require less insulin or fewer meds (hopefully none) to control your diabetes.
In the past 10 to 15 years the recommendations on how duration and frequency of exercise have changed. The 12 to 15 minutes 3 times per week felt to be sufficient 15 yrs ago has been increased to at least 30 min 4 to 5 times per week. I feel that each day should include physical activity of at least 30 min duration. It requires effort but as aforementioned, the benefits are soon recognized and long lasting.
Contact my office for an appointment if you’d like to start an exercise program and don’t know where to begin.
WEIGHT LOSS
Losing weight is easier than you think!

With the rise in obesity in our society (and the world), weight loss has become a very hot topic. I am frequently asked by family and friends to give my opinion on which diet is most effective. My answer is usually the same: eat less and exercise more. The reasons we gain weight are multiple. While glandular issues and certain medications can result in weight gain, this is infrequently the cause. In most cases, excess weight is gained due to positive net energy. Think of food (calories) as energy. If you consume more energy than you expend (or “burn”), energy is stored. (You wouldn’t fill your gas tank with more fuel than it can hold. Think of your body in the same way.) This storage of energy is in the form of fat. While we all must retain a percentage of fat as energy reserve for periods of decreased food intake and for temperature regulation, excess fat is termed overweight, obesity, or morbid obesity depending on the body fat percentage and/or weight over ideal body weight. On the contrary, when we expend (“burn”) more energy/calories than we consume, the result is a negative net energy: this results in weight loss.
Equally important is what we consume. Carbohydrates are quick energy sources which do not provide long term satiety (feeling satisfied or no longer hungry). Examples of carbohydrates are bread, rice, sweets, fruits. Examples of “good carbs” are whole wheat, grains, “healthy” cereals, fruits, beans. Examples of “bad carbs” are white bread and rice, most sweets (chocolate, candy, cake. donuts), and soft drinks. Fats and proteins are more difficult to digest and provide a longer lasting satiety. They result in a slower and more prolonged rise in blood sugar to be used by the body for metabolism (resting body functions) and activity (walking, standing, bathing, dressing, exercise, etc.). Examples of proteins are beef, chicken, seafood, nuts, soy products. Examples of fats are butter, oil, and margarine. Most foods contain carbohydrates, proteins, and fats. The key is to eat foods and meals which consist of low fat, modest protein and carbohydrates. Beware of low fat and no fat foods: they still have calories. Hi fat foods (fast food), sweets, soft drinks should only be consumed occasionally: definitely not daily!
Losing weight is more simple than advertisers and diet plans would have you believe. Eat less. Eat smarter. Exercise more. Plan your meals accordingly and keep healthy snacks such as nuts and whole grain crackers and bread so you don’t get hungry on the run and succumb to the pressures of the ever so available fast food. Incorporate exercise into your daily routine and try to avoid doing things the easy way.
Remember these tips and you’ll be well on your way to sustained weight loss and a healthier life. You can do it!
STROKE
What is a stroke?
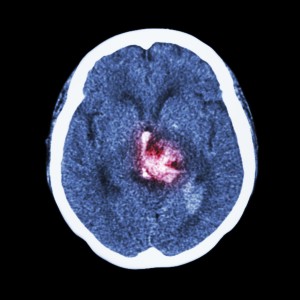
Stroke is one of the leading causes of permanent disability. A stroke occurs when there is a sudden loss of blood flow (perfusion) to a part of the brain. This can be due to a blockage (ischemic) or a bleed (hemorrhagic): the sequelae are the same. A stroke (cerebrovascular accident, or CVA) can affect vision, balance / coordination, speech, comprehension, expression, emotion, swallowing function, sensation to touch, movement of arms and legs (typically on one side), and bowel / bladder function. What is affected depends upon the location of the stroke, volume of infarcted (irreversibly damaged due to insufficient blood flow) tissue and duration of initial stroke symptoms. The duration is important because if taken to the hospital within 3 to 4.5 hours of the onset of symptoms, patients with an ischemic (non-bleeding) stroke may be candidates for thrombolytic (“clot-busting”) therapy, which may reverse stroke symptoms.
IF A PERSON DEVELOPS THE SUDDEN ONSET OF SLURRED SPEECH, CONFUSION, INABILITY TO WALK, TALK, OR MOVE A LIMB, THAT PERSON SHOULD BE TAKEN IMMEDIATELY TO THE NEAREST EMERGENCY DEPARTMENT BY EMERGENCY MEDICAL SERVICES.
Typically, stroke results in impaired speech, difficulty swallowing, difficulty or inability moving the upper and or lower limb. The result is impaired communication, nutrition, ambulation, and ability to perform typical self-care tasks, or activities of daily living (ADLs). There is therefore a loss of independence. Incontinence of bowel and bladder may occur and typically improves. Other causes of incontinence such as urinary tract infection and or excessive laxatives / stool softeners or diarrhea associated with antibiotic use should be ruled out as these are reversible causes of incontinence. Occasionally medication is used to improve urinary incontinence. Bowel and bladder scheduling / retraining is particularly helpful. Incontinence is of major concern because it can be a significant determinant on whether or not a patient’s family is able to provide care at home.
Occasionally stroke can result in increased muscle tone in the affected limb (spasticity), which may result in limb contracture. This should be addressed early to prevent permanent contracture. Bo-Tox administration and therapy (occasionally casting or splinting) are indicated for this with good results. Persons with stroke may also develop depression: this is more common in those with dominant hemisphere involvement (typically on the left). This is more common in those with a history of depression. Antidepressants are helpful, as depression has been shown to negatively affect stroke outcomes in spite of rehabilitation efforts.
Rehabilitation early after stroke is extremely important and has been shown to improve outcomes. The first couple of months after stroke are crucial for aggressive rehabilitation efforts as this is the period of increased neuroplasticity (a sort of brain tissue remodeling). Inpatient rehabilitation hospitals offer the greatest benefit due to the intensive multidisciplinary approach to stroke recovery. This setting offers oversight and daily visits by the rehabilitation physician, PT, OT, and Speech therapies, neuropsychologist testing and counseling, 24 hour rehab nursing care, and social work coordinating care both during and after the admission.
The risk factors for stroke include family history, previous stroke, high blood pressure, diabetes, high cholesterol, recent cardiovascular surgery, stimulant abuse, steroid use (increased along with tobacco abuse), to name a few. If these factors are present, exercise, diet modification to improve blood sugar control and lower cholesterol, stress management, cessation of tobacco, and stimulant abuse can reduce the risk of stroke.