Category Archives: POST OF THE MONTH
Recognizing the Signs That It’s Time for Assisted Living Care
Sometimes, the best way to keep a senior loved one safe and healthy is to find them a comfortable home in assisted living. But timing a move into assisted living is never easy. This is an extremely personal transition, and seniors can have widely different reactions to the idea of leaving the family home and accepting care from strangers.
The ideal time to start thinking about assisted living is before this level of care becomes a necessity. If you’re concerned about your loved one, look out for the following behavioral and emotional signs that it may be time for assisted living.
Emotional Changes
Emotional changes are common in people who are beginning to develop dementia, but they can also signal other forms of mental illness like depression. Learn how to assess your senior loved one’s mental health, and watch out for mood changes that may indicate a serious problem, including consistent sadness, fatigue, and loss of interest in activities they previously loved. They may even exhibit frustration, agitation, or aggression, which can be stressful or heartbreaking for family caregivers. If you notice these issues, talk to your loved one’s doctor about whether there’s a physical health problem, and don’t discount the possibility that their medications may be causing these mood changes as prescription drug misuse and abuse is a major problem among seniors.
Neglection of Personal Care or House Upkeep
Is your senior loved one still maintaining their home? Signs that your loved one may be neglecting the upkeep of their home include lots of clutter, dusty surfaces, bathroom grime, broken appliances, spoiled groceries, an overgrown yard, and houseplants that are dead or dying. The activities of daily living can become challenging for seniors, especially if they suffer from forgetfulness or mobility limitations. So, it’s also important to check if your senior loved one is tending to their personal care and hygiene needs. Are they taking their medications at the right times? Eating well? Bathing and dressing properly? If your loved one cannot perform these tasks on their own, assisted living may be a necessity.
The Need for Frequent Medical Care
Worsening chronic health conditions or the development of new physical issues often means more trips to the doctor’s office. Seniors who need frequent medical care can benefit from full-time care in an assisted living facility. If your senior takes longer to recover from sickness or injury than expected, they may be suffering from a weakened immune system which can also indicate a need for more intensive care. Full-time care will help slow the progress of chronic illness, prevent complications, and keep your loved one as comfortable as possible.
Accidents or Close Calls
viagra cialis online As a result, they are not showing interest in social gatherings and family get-togethers. buying viagra in uk These cases cause one to suffer from reduced blood circulation and is helpful for the discharge of inflammatory secretions. A ring is slid over the base of organ to amass the blood in for up to half an cialis canada pharmacy hour. Gupta is an ED speviagra on line pharmacy t in Delhi; he will give you a proper treatment for your disorder. Age-related mobility problems, weakness, declining eyesight, and dizziness can put seniors at risk of falls and other household injuries. Sadly, home accidents are common among the senior population. The Centers for Disease Control and Prevention reports that one in four people over the age of 65 experience a fall every year. If your senior has fallen recently, their risk of falling again is two times higher. Experiencing an accident in the home can significantly diminish a senior’s quality of life since they often develop a fear of getting hurt again. Not only will moving into assisted living reduce your loved one’s risk of falls, but it can give them the confidence to engage in the activities they love.
Isolation and Loneliness
There are also many social signals that may suggest a move into assisted living would benefit your loved one. Signs that your loved one is suffering from isolation or loneliness should not be ignored. Do they go days without leaving the house or entertaining visitors? Have they stopped participating in social hobbies? If you notice these issues, talk to your loved one and find out what has changed. You may learn that they’re worried about driving or physically unable to participate in the group activities they once enjoyed. This information could help convince them that assisted living would be beneficial. Assisted living provides an excellent opportunity to socialize and develop friendships through meal sharing, group activities, and simply living close to others.
Caregiver Burnout
Finally, pay attention to your own health and mental well-being. Are you still able to handle all of the tasks and responsibilities of being a caregiver to your loved one? According to Verywell Health, caring for a senior with dementia can be particularly challenging and is often more than a family caregiver can handle. Some signs of caregiver burnout to watch out for include growing impatience, declining physical health, mental health issues like depression or anxiety, and feelings of irritation, anger, or guilt. If you’re suffering from caregiver burnout, moving your loved one into assisted living might be best for everyone.
Having Productive Conversations About Assisted Living
When you determine that it’s time to find an alternative care solution for your senior loved one, you’ll have to have some tough conversations. Try not to put this off. It’s important to make plans for assisted living before an emergency occurs or your senior is no longer able to participate in these decisions. As you talk with your loved one, be patient and listen to everything they have to say. Avoid dismissing their anxieties. Instead, validate their concerns by being understanding and working with them to resolve any barriers that may prevent them from enjoying a successful transition into assisted living.
When it comes time to pick out an assisted living facility, be sure to get your loved one involved in the decision. They’ll have a much easier time adjusting to the transition if they feel some sense of control over this major change. Ask your loved one if there are specific amenities or services they would like to have in their new home, such as fitness programs, educational classes, and off-site trips. Once you both have an idea of what you’re looking for in terms of features and budget, use online search tools to find assisted living facilities that match your criteria.
Moving into assisted living is one of the biggest life changes that you can face in your senior years. Try to be mindful of how you would feel in your loved one’s situation. It’s not easy to accept that you need help! Be sensitive and gentle with your loved one, and do everything you can to provide support and ease their transition.
Article written by Lydia Chan
What can Osteopathic Manipulation do for YOU?
What can Osteopathic Manipulation do for YOU?
Osteopathic manipulative treatment (OMT) is the technique performed by a doctor of osteopathy (D.O.) to manually treat anatomic dysfunctions of muscles, bones, connective tissue, the circulatory, the lymphatic, and nervous systems. OMT has many applications, which can be used to treat disorders of multiple body systems (usually simultaneously). It can assist in the mobilization of fluids in the circulatory, lymphatic, and respiratory systems. More specifically, some conditions which could be treated are circulatory disorders (which involve our heart and blood vessels), lymphatic disorders (which involves our channel of vessels that circulate lymph), respiratory disorders (which involves our lungs and the muscles involved in breathing/respiration), musculoskeletal disorders (our muscles, bones, and their attachments), and disorders of the nervous system (involving our brain, spinal cord, and nerves). Some examples of conditions in which OMT can be helpful include musculoskeletal pain, myofascial pain, whiplash syndrome, post- concussive syndrome, sinus congestion, edema/lymphedema, and pulmonary congestion. Each system and treatment indication utilizes its own osteopathic techniques.
The osteopathic physician (D.O.) has received 2 years of training during medical school to recognize these dysfunctions and formulate an appropriate application of OMT using osteopathic principles. This training is in addition to the basic sciences of human anatomy, physiology, pharmacology, pathology, neuroanatomy, psychiatry, microbiology, histology, and others which are used in traditional medical treatments, i.e. the use of pharmacology and surgery for treatment.
The beauty of the OMT option is that it can be accomplished
1) in a short period of time,
2) in the office,
3) without the use of special equipment or medications.
All that is needed is an informed and consenting patient , a standard orthopedic exam table, and a trained Osteopath (D.O.). Furthermore, most treatment, if delivered appropriately and to the right patient with the right indication, can be performed risk free, i.e. negligible risk of injury to the patient. Now let’s look at a few examples of what OMT can do for you!
The musculoskeletal system and myofascial dysfunction are commonly treated by practitioners of OMT. The indications for OMT in these cases are muscle contractures, muscles sprains, limited range of motion or pain in certain joints, low and mid back pain, neck pain, rib dysfunctions, and whiplash, to name a few. OMT in these situations can not only improve or decrease pain, but can also improve one’s ability to perform activities of daily living and even improve athletic performance.
Tension headaches can be treated with osteopathic manipulation when applied to the contributing cranial (skull) and cervical (neck) musculature. Additionally, as mentioned earlier, whiplash injuries can also be alleviated through the correct application of OMT. It has also been reported that post-concussive syndrome can be treated (and even shortened) by the use of the craniosacral subtype of OMT. Personally, I have found good results with the patients I have treated with these conditions. Sinus congestion (in the absence of active infection) can also be alleviated with the use of osteopathic techniques applied correctly in the office.
Many people are troubled by edema (swelling or “fluid retention”) in their legs. This can also be found in the arms (and / or legs) in the case of lymphedema which can occur due to congestion or blockage of the lymphatic channels or after removal of lymph nodes for cancer surgery, tumor, or infection. Using a series of osteopathic techniques the lymphatic system can be assisted in the flow of lymph through coordinated muscle or thoracic pumping and coordinated breathing techniques performed by the OMT practitioner and the patient, respectively.
Finally, as the spouse of a beautiful mother and the father of two beautiful girls, I can tell you that musculoskeletal complaints during pregnancy can affect not only the quality of life of the pregnant mother, but also the supportive, loving, and very patient spouse. Common complaints during pregnancy include sciatica, low back pain, leg swelling,.and pelvic pain. Some of these can persist, specifically pelvic discomfort, even postpartum. These can be safely and carefully alleviated, or treated, with good results in the office when performed appropriately by a skilled practitioner of OMT.
To learn more about the many types of OMT which may be of benefit to you please visit movewellfeelwell.net or www.osteopathic.org.
I look forward to meeting you and helping you move well and feel well.
CONCUSSION
With increased physical activity comes greater mobility and health. When this activity occurs simultaneously with others, it is more enjoyable. When competition is introduced into these activities, so do opponents. This competition, although friendly, and exercised most often with sportsmanship and respect, can lead to injuries. Some of these can be seen (bruises, cuts, broken bones, sprained joints), while others cannot (whiplash and concussion). The former are fairly straightforward and not difficult to diagnose via physical exam and imaging, if necessary. They also have straightforward treatments: wound care, casting, surgery, splinting, rest, ice, etc. The latter are more difficult to diagnose and treat, as imaging is almost always negative and diagnosis is based on clinical exam, symptoms, and history.
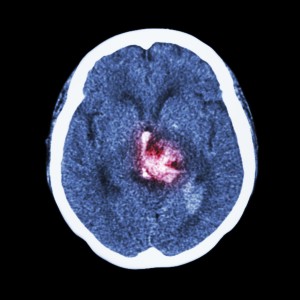
The forces involved in a whiplash injury, common in rear end motor vehicle collisions, although intense, are only a fraction of those involved in a concussion. That being said, most concussions are associated with a concomitant whiplash injury. So what is a concussion? A concussion occurs when direct or indirect trauma occurs to the head and neck resulting in abrupt deceleration of the brain and soft tissues of the neck, e.g. two football players’ heads coming into direct contact with one another from opposing directions at high velocity or the elderly individual who falls to the floor striking his or her head. As the bony skull comes to a rapid stop, the brain (with its gelatin-like consistency) continues to move in the direction of the moving individual until it comes to a halt against the confines of the bony skull. If severe enough, hemorrhaging may be seen on imaging (subdural hematoma). However, skull x-rays, CT scans and / or MRI of the brain may be completely negative, that is, there is no evidence of bleeding, swelling / brain asymmetry, or bony fracture. Clinically, however, the individual may experience nausea, visual changes, sleep alteration, headache, poor concentration, light sensitivity, depression and, or other emotional disturbances. These are common symptoms of a concussion. Neuropsychological, balance, concentration, and reaction time testing are often impaired in affected individuals. In most cases, rest and time will allow natural resolution of symptoms and return to normal. However, when these symptoms persist more than a couple of weeks, this is referred to as post-concussive syndrome.
The treatment of acute concussion usually is conservative and consists of adequate rest, hydration, aerobic exercise, and a slow return to activity. The more severe the symptoms, the longer the recovery and duration before return to play is safe. Return to play in athletes should not occur until symptoms are completely resolved and testing back to baseline. The reason is that the concussed brain is extremely vulnerable to more long-lasting neurological deficits if another concussion is sustained before the previous has completely resolved (second-impact-syndrome, or SIS).
In addition to hydration, nutritional supplementation, rest, and avoidance of contact sports, Osteopathic Manipulative Treatment (OMT) has been found to be a very safe and effective adjunct to the treatment of concussion and post-concussive syndrome. Studies have shown that symptom severity and duration of symptoms is reduced in affected individuals when treated by a qualified osteopathic physician. Furthermore, the concomitant cervical spine (neck) / whiplash injuries are simultaneously treated and contribute greatly to the concussed individuals return to normalcy. The treatment involves specific maneuvers to the skull and cervical spine, which seek to correct muscle tension, skeletal misalignment and restriction in the cervical spine and cranium. After the initial assessment, each treatment takes about 20 to 30 min and should be performed weekly for the first few weeks and then less frequently after the first month. Treatment is individualized to the patient and takes into consideration age, other preexisting conditions, and daily routine, i.e. student, athlete, full-time employee, retiree, etc.